Special Interest Group Update
In each issue, one of NANN's special interest groups shares information in their area of focus.
Back to Basics: Blood Groups and Blood Screening
Tosha Harris, DNP APRN NNP-BC, NANN E-News editor
Blood groups, also known as blood types, refer to the classification of human blood based on the presence or absence of specific antigens on the surface of red blood cells.
The Working Party for Red Cell Immunogenetics and Blood Group Terminology of the International Society of Blood Transfusion (n.d.) recognizes 44 blood group systems; the two most significant group system are the ABO and the Rh blood group systems.
ABO Blood Group
The ABO blood group system is based on the presence or absence of two antigens, A and B, on the surface of red blood cells and corresponding antibodies in the plasma. Antigens are molecules or molecular structures that can trigger an immune response in the body.
Typically, antigens are foreign substances like bacteria, viruses, fungi, and parasites. However, antigens also can be present on the surface of cells, including red blood cells, and they are essential for determining blood type in the ABO blood group system. When the immune system encounters an antigen, it recognizes it as foreign and mounts an immune response to eliminate or neutralize it. Antigens help the immune system distinguish between self (the body's cells and molecules) and nonself (foreign invaders) to protect the body from harmful pathogens. The antigens of the ABO blood group are sugars, and the antigens of the Rh blood group are proteins (Dean, 2005a).
Antibodies, which are immunoglobulins mainly of the IgM class, are proteins produced by specialized white blood cells called B lymphocytes (B cells). They are an essential part of the adaptive immune response and are formed naturally. When an antigen enters the body, B cells recognize it and produce specific antibodies that can bind to that antigen. Other immune system components target the antigen for destruction by attaching themselves to their targeted antibody.
B cells also play a crucial role in immune memory. After an initial encounter with an antigen, B cells can develop memory cells that "remember" the antigen. If the same antigen appears in the future, the immune system can mount a faster and more effective response, preventing the infection from causing significant harm.
There are four main blood types in the ABO blood group system: A, B, AB, and 0.
Table 1.
ABO Blood Group System Types
|
Blood Type |
Antigen on RBC |
Antibody in Plasma |
Rh Factor |
|
A |
A |
Anti-B |
+ or - |
|
B |
B |
Anti-A |
+ or - |
|
AB |
A and B |
None present |
+ or - |
|
O |
None present |
Anti-A and Anti-B |
+ or - |
Note. RBC = red blood cell; Rh = Rhesus.
Rh Blood Group
The Rh blood group system, also known as the Rhesus system, is one of the most critical and well-known blood group systems in human blood typing. The Rh system categorizes blood by the presence or absence of a specific antigen known as the Rh factor—or the D antigen—on the surface of red blood cells. Because red blood cells lacking the Rh antigen have an abnormal shape, these antigens are believed to help maintain the integrity of the red blood cell membrane (Dean, 2005b). If a person's red blood cells have the Rh antigen, they are classified as Rh-positive (Rh+). If their red blood cells lack the Rh antigen, they are classified as Rh-negative (Rh-). Weak or partial D antigens may present in newborns born to D-negative (Rh-) mothers due to reduced antigenic sites or the loss of extracellular D epitopes (Li & Guo, 2022).
Figure 1.
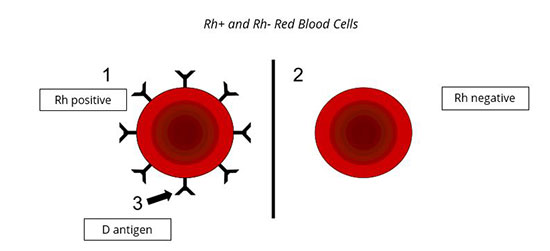
Note. “Red blood cells drawing.svg” by Sophiedionne14 is adapted and licensed under CC BY-SA 4.0. 1 = Rh-positive red blood cell; 2 = Rh-negative red blood cell; 3 = the D antigens that make the red blood cell Rh-positive.
ABO Incompatibility
ABO incompatibility is a condition that occurs when there is a mismatch between the ABO blood group of a mother and her fetus during pregnancy or between blood donor and recipient during blood transfusion.
The most common type of ABO incompatibility during pregnancy occurs when a mother with blood type O carries a fetus with blood type A or B. The mother's immune system recognizes the A and B antigens on the fetal red blood cells as foreign and produces antibodies against these antigens. These antibodies can cross the placenta to attack the fetal red blood cells, causing hemolysis (destruction of red blood cells) and potentially leading to hemolytic disease of the newborn (HDN) or erythroblastosis fetalis.
The most common clinical manifestations of ABO incompatibility seen in neonates are anemia, reticulocytosis, and jaundice. Infants who undergo phototherapy or receive an exchange transfusion to treat the results of the ABO incompatibility may experience an exaggerated physiologic anemia nadir at 8–12 weeks (Gomella et al., 2020).
Rh Incompatibility
Rh blood group identification is essential during pregnancy and before blood transfusions. An Rh-negative person exposed to Rh-positive blood may develop antibodies against the Rh antigen (Rh sensitization), causing problems in subsequent transfusions or with Rh-positive blood.
Rh sensitization is particularly concerning during pregnancy when an Rh-negative mother carries an Rh-positive fetus. In such cases, the mother's immune system may produce antibodies against the Rh antigen, potentially leading to hemolytic disease of the newborn (HDN) in subsequent pregnancies with Rh-positive babies. HDN can result in severe anemia, unconjugated hyperbilirubinemia, hepatosplenomegaly, hydrops fetalis, and even death (Gomella et al., 2020).
To prevent Rh sensitization during pregnancy, Rh-negative pregnant women may receive an injection of Rh immunoglobulin (RhIg or RhoGAM) at specific times during pregnancy and after childbirth. Rh immunoglobulin helps prevent the mother’s immune system from producing antibodies against the Rh antigen and reduces the risk of HDN in future pregnancies.
Blood Screening
The direct antiglobulin test (DAT), type and screen, and type and crossmatch are important tests performed on newborn babies to assess their blood compatibility and potential risk of HDN during the perinatal period. Each test serves a specific purpose in the management of neonatal blood compatibility.
A DAT is performed to identify maternal antibodies already attached to the baby’s red blood cells. The neonatal type and screen helps determine the baby's blood group and screen for unexpected antibodies, and the neonatal type and crossmatch ensures compatible donor blood is available for transfusion if required. These tests collectively aid in appropriately managing neonatal blood compatibility and preventing HDN and other transfusion-related complications.
Direct antiglobulin test. The direct antiglobulin test (DAT), or direct Coombs test, is performed to detect the presence of maternal antibodies on the neonate's red blood cells. The DAT test involves taking a blood sample from the neonate and adding a Coombs reagent to the sample. If the red blood cells agglutinate (clump), it indicates a positive result, suggesting maternal antibodies coated the baby's red blood cells. A positive DAT may warrant further investigation and intervention to manage HDN.
Type and screen. The neonatal type and screen test is typically performed when there is a known risk of ABO or Rh incompatibility, elevated unconjugated hyperbilirubinemia occurs within the first 24 hours of life, or if there is a potential need for surgery. This test determines the neonate's blood type and screens for antibodies in their blood. The neonatal type and screen process typically involves determining the newborn's blood type and Rh blood type (‘type’)and screening for atypical plasma antibodies (‘screen’). These antibodies may have developed in response to exposure to foreign blood types from the mother during pregnancy.
Type and crossmatch. The blood crossmatch is performed after the initial type and screen, which determined the neonate's ABO and Rh blood group, and identified any unexpected antibodies in their plasma. With this information available, the crossmatch is conducted to minimize the risk of adverse reactions caused by transfusing incompatible blood.
- Major crossmatch: For this procedure, a small sample of the potential donor’s red blood cells is mixed with a sample of the recipient’s plasma (the liquid component of blood containing antibodies). This mixture is observed for agglutination (clumping) or hemolysis (destruction of red blood cells). Agglutination or hemolysis indicates an incompatible match between the recipient’s antibodies and the donor’s red blood cells.
- Minor crossmatch: A minor crossmatch may be performed if necessary. This involves mixing a small sample of the donor’s plasma (serum) with the recipient’s red blood cells. The mixture is observed for agglutination or hemolysis, either of which would indicate incompatibility between the donor’s antibodies and the recipient’s red blood cells.
Determining a neonate's blood type and compatibility is critical for identifying potential risks and providing optimal care during the perinatal period. Early detection of blood incompatibility enables neonatal care providers to take preventive measures and avoid serious complications such as HDN, transfusion reactions, and Rh sensitization.
References
Dean, L. (2005a). Blood groups and red cell antigens. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK2264/#ch2.1.2
Dean, L. (2005b). Blood groups and red cell antigens. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK2269/
Gomella, T. L., Eyal, F. G, & Bany-Mohammed, F. (Eds.). (2020). Gomella's neonatology: Management procedures, on-call problems, diseases, and drugs (8th ed.). McGraw Hill. https://accesspediatrics.mhmedical.com/content.aspx?bookid=2762§ionid=234449598
International Society of Blood Transfusion (n.d.). Red cell immunogenetics and blood group terminology. https://www.isbtweb.org/isbt-working-parties/rcibgt.html#:~:text=The%20International%20Society%20of%20Blood%20Transfusion%20(ISBT)%20Working%20Party%20for,cell%20antigens%20(December%202022).
Li, H. Y., & Guo, K. (2022). Blood group testing. Frontiers in Medicine, 9, 827619. https://doi: 10.3389/fmed.2022.827619
Join the discussion on the MyNANN Advanced Practice SIG forum.


