Special Interest Group Update
In each issue, one of NANN's special interest groups shares information in their area of focus.
Syphilis and Congenital Syphilis: A Review
Tosha Harris, DNP APRN NNP-BC
Education SIG
Sexually transmitted diseases (STDs) are at an all-time high. More than 2.5 million cases of chlamydia, gonorrhea, and syphilis were reported in 2019 in the United States. 2019 marked the sixth consecutive year of increased reported cases of STDs (Centers for Disease Control and Prevention [CDC], 2021a).
These increases are a concern for those caring for neonates, who can acquire STDs like syphilis from their infected mother during pregnancy. The diagnosis and treatment of infants exposed to syphilis is dependent on identifying maternal infection during pregnancy or at delivery. Currently, most states have legislation that requires universal maternal screening of all pregnant women at least once during their pregnancy. However, less than half of these states have laws that require screening in the third trimester, and only 11 require screening at delivery (CDC, 2021b). A thorough review of maternal prenatal history should be a high priority, particularly in western and southern states where congenital syphilis rates are high (CDC, 2021a).
Syphilis is caused by the bacterium Treponema pallidum, a thin, corkscrew-shaped, flagellated, motile, gram-negative spirochete (Easterlin, et al., 2021). Humans are the bacteria’s only natural host, and transmission is usually through sexual contact with an infected person. T. pallidum is highly contagious, and the risk of transmission is estimated to be 50% to 60% from a single unprotected sexual exposure (Duff, 2021). Common entry points are through mucosal surfaces like the genital organs (e.g., penis, vagina, cervix) and the anus, lips, breasts, and tongue (Dobson & Sanchez, 2019). Due to the organism’s fragile nature, survival outside of the body is limited; however, clinicians may become infected by contact with lesions if personal protective equipment is not utilized and contact is made through abraded areas of the skin (Dobson & Sanchez, 2019).
Acquired Syphilis
Inside the body, T. pallidum multiplies and quickly spreads through the lymphatic system and into the systemic circulation. The incubation period averages 21 days but can range from 10–90 days (Duff, 2019).
Primary Syphilis
Following spirochetemia, the infected person enters the primary stage of syphilis. This stage is characterized by a painless chancre that occurs at the spirochetes’ point of entry. The chancre is easily recognizable in men, but can be easily missed in women without a thorough pelvic examination because the chancre may be located on the cervix or in the vagina.
Only a single chancre is present in most cases, but multiple chancres can occur if concomitant infections such as HIV are present. Localized lymphadenopathy is often present. Even without treatment, the chancre usually will spontaneously resolve in 3–6 weeks (Adhikari, 2021; Heresi, 2017; Kollman & Dobson, 2016).
Secondary Syphilis
Six to eight weeks the chancre heals, the classic symptoms of secondary syphilis appear. The most common symptom is a diffuse maculopapular rash that begins on the trunk and extremities and spreads over the entire body, including the palms and soles of the feet, except for the face. Oral mucosal lesions appear as white patches or plaques on the dorsal and ventral surfaces of the tongue, soft palate, and pillars. Condylomata lata can occur in the anal or vaginal area.
Other nonspecific symptoms that can occur during this phase include malaise, fever, sore throat, headache, arthralgia, alopecia, and generalized lymphadenopathy. All lesions associated with secondary syphilis are highly contagious. Regardless of treatment, symptoms usually resolve within 3-12 weeks (Adhikari, 2021; Dobson & Sanchez, 2019; Duff, 2019; Heresi, 2017; American Academy of Pediatrics [AAP], 2018; Kollman & Dobson, 2016).
Latent Syphilis
During this infection period, the infected individual will be seroactive but have no identifiable infection signs. Based on the timing of initial exposure and symptom manifestation, people with latent syphilis are subdivided into two categories:
- early non-primary, non-secondary syphilis (also known as “early latent”; <1 year after infection)
- late latent (>1 year after infection or unknown duration; Adhikari, 2021; Heresi, 2017).
Tertiary Syphilis
The tertiary stage of syphilis occurs approximately 15–30 years after initial infection and is rare in reproductive-aged women and developed countries (Adhikari, 2020; Phillippi, 2015). Without treatment, one-third of infected people will advance to tertiary syphilis (Duff, 2021; Heresi, 2017).
Pathognomonic symptoms of tertiary syphilis include gummata (soft- tissue tumors that cause extensive necrotic damage), aortic valve disease, aortic aneurysm, and aortic insufficiency. Another characteristic sign of tertiary syphilis is the Argyll Robertson pupil, which means the pupil reduces in size to view a near object (accommodate) but not in reaction to bright light (Duff, 2019, 2021; Phillipi, 2015).
Neurosyphilis most commonly occurs in the later stages of infection but can occur at any stage if the individual is HIV positive. It can affect the brain, eyes, joints, bones, and heart. Signs of nervous system involvement include headache, altered behavior and mood, meningitis, uveitis, seizures, dementia, and tabes dorsalis (a high-stepping gait with the feet slapping the ground with each step due to a loss of proprioception) (Collins Fantasia & MacIntyre, 2019; AAP, 2018).
Testing
The CDC and the U.S. Preventive Task Force recommend screening for syphilis during pregnancy at all patients’ first prenatal visit. Repeat testing at 28 weeks and delivery is recommended for women who have positive initial screens, are at high risk for treatment failure and reinfection, or who live in communities with high infection rates (Workowski et al., 2021; U.S. Preventive Services Task Force, 2018).
Antepartum screening for syphilis is a two-step process that uses one of two screening approaches: the conventional method and the reverse sequence screening method.
The first screening approach is the conventional method shown in Figure 1. The conventional approach entails performing a nontreponemal antibody test (rapid plasma reagin [RPR] or venereal disease research laboratory test [VDRL]), followed by a confirmatory treponemal antibody test (i.e., fluorescent treponemal antibody absorption test [FTA-ABS], T. pallidum particle agglutination [TP-PA], T. pallidum chemiluminescent assay [TP -CIA], or T. pallidum enzyme immunoassay [EIA]) (CDC, 2021a; AAP, 2018, U.S. Preventive Services Task Force, 2018).
Nontreponemal tests (NTT) help monitor syphilis infections and responses to therapy. These tests detect the IgG and IgM antibodies to cardiolipin released by the syphilitic infected host cells (Easterlin et al., 2021). The tests are sensitive but not specific to syphilis antibodies; false positives can occur in the presence of viral infections, tuberculosis, lymphoma, connective tissue diseases, intravenous drug use, and pregnancy (Easterlin et al., 2021; Collins Fantasia & McIntyre, 2019).
Figure 1
Conventional Testing Algorithm
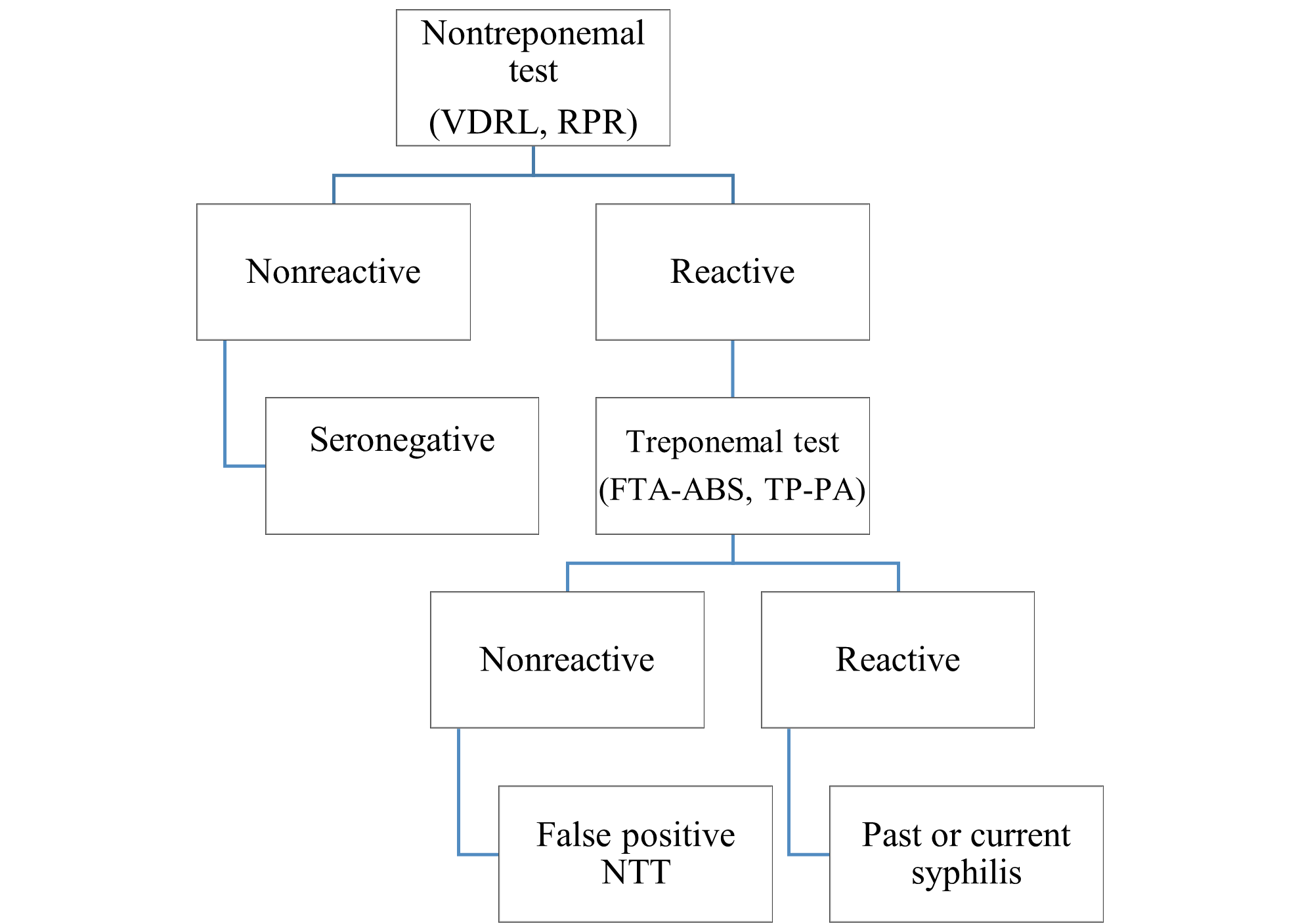
Adapted from American Academy of Pediatrics (2018). Syphilis. In D. W. Kimberlin, M. T. Brady, M. A. Jackson, & S. S. Long (Eds.), Red book: 2018 report of the committee on infectious diseases (31st ed., pp. 773-787).
The second screening method—which is faster and less expensive than the conventional screening—is the reverse sequence screening method shown in Figure 2. The treponemal antibody test (TT) is performed first, followed by a nontreponemal test. A second treponemal test is performed if the test results are discrepant (Workowski et al., 2021; U.S. Preventive Services Task Force, 2018). Treponemal tests, in contrast to nontreponemal tests, are specific to T. pallidum antibodies. False positives can occur if other spirochete infections, such as Lyme disease, are present (Easterlin et al., 2021).
Figure 2
Reverse Sequence Screening Algorithm
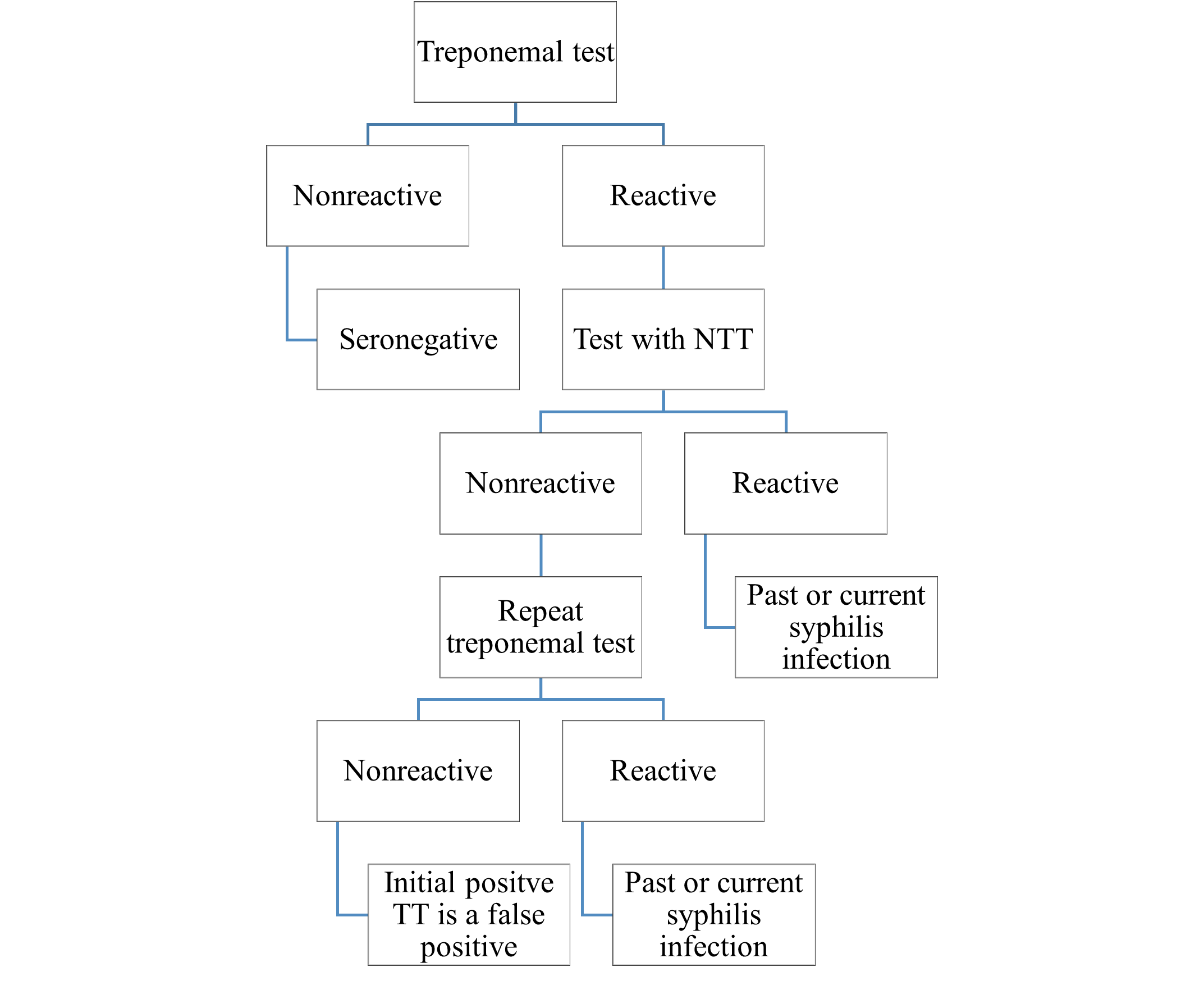
Adapted from American Academy of Pediatrics (2018). Syphilis. In D. W. Kimberlin, M. T. Brady, M. A. Jackson, & S. S. Long (Eds.), Red book: 2018 report of the committee on infectious diseases (31st ed., pp. 773-787).
Treatment
The CDC (2021a) has published guidelines for the treatment of syphilis. For this article, only treatment in pregnant women will be discussed. Treatment of syphilis infections is based on the stage of infection, as shown in Table 1. Parenteral penicillin is the only medication proven to prevent vertical transmission of syphilis to the baby. Mothers with sensitivity to penicillin should be desensitized, then treated (Workowski et al., 2021). Alternative treatment medications, such as doxycycline and tetracycline, are contraindicated during pregnancy but can be used by women who aren’t pregnant and are allergic to penicillin (AAP, 2018).
Table 1
Treatment of Syphilis During Pregnancy
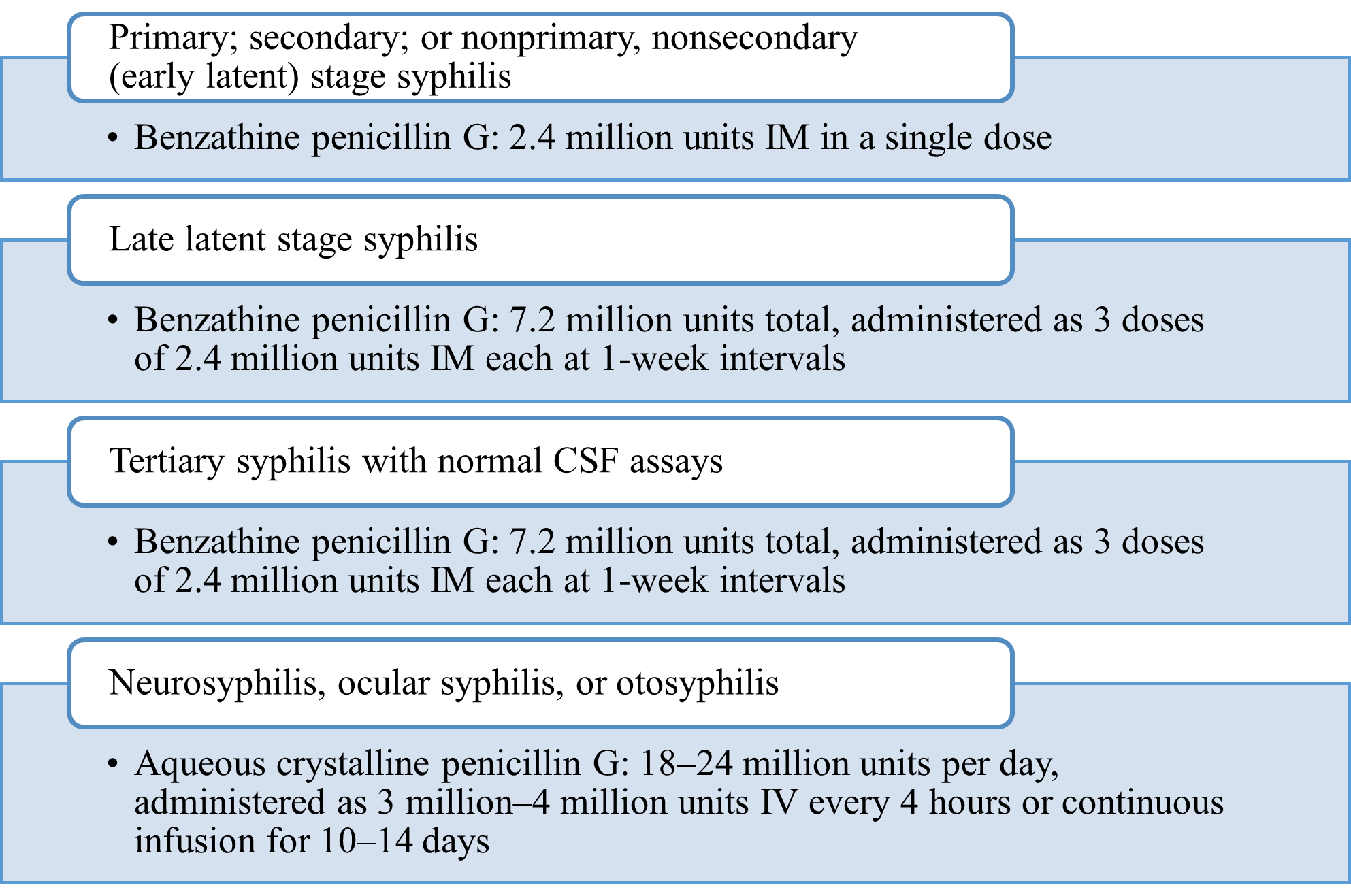
Adapted from Workowski, K. A., Bachmann, L. H., Chan, P. A., Johnston, C. M., Muzny, C. A., Park, I., Reno, H., Zenilman, J. M., & Bolan, G. A. (2021). Sexually transmitted infections treatment guidelines, 2021. MMWR. Recommendations and Reports, 70(4), 1–187. https://doi.org/10.15585/mmwr.rr7004a1
Mothers treated for syphilis during pregnancy should be tested for other sexually transmitted infections, particularly HIV. Monthly follow-up and repeat testing, according to state regulatory guidelines, should be provided. A fourfold decrease in nontreponemal titers should be expected with successful treatment; an increase in titers from pretreatment levels indicates reinfection or treatment failure (Easterlin et al., 2021; Heresi, 2017).
Congenital Syphilis
Transplacental transmission is possible during pregnancy and delivery at any stage of maternal syphilis infection. Syphilis can be transmitted as early as 6-–9 weeks gestation though the risk of transmission increases as the pregnancy advances (Duff, 2021; Micheals et al., 2018). A direct correlation exists between vertical transmission and the maternal stage of syphilis (Kollman & Dobson, 2016).
Congenital syphilis (CS) rates mirror rates of primary and secondary infection rates in women. From 2018 to 2019, congenital syphilis increased 41.4% (34.3-–48.5 per 100,000 live births), equaling 1,870 cases of congenital syphilis. This increase coincided with a 27.9% (6.8–8.7 per 100,000) increase in primary and secondary syphilis rates among women ages 15-44 years (CDC, 2021a). Mothers in the primary or secondary stage of syphilis have a 50% risk of transmitting syphilis to their fetus. Later stages of syphilis infection, such as early latent and late latent, carry a 40% and 10% risk, respectively (Duff, 2021).
According to the CDC (2021a), maternal risk factors for contracting syphilis during pregnancy include sex with multiple partners or in exchange for money; lack of prenatal or late prenatal care; use of illicit drugs, incarceration of the woman or her partner, and unstable housing or homelessness. Black and Hispanic women are at higher risk of contracting syphilis than their non-Hispanic White counterparts (CDC, 2021a).
Transplacental transmission of syphilis can result in non-immune hydrops, preterm birth, low birth weight, and fetal and neonatal death (Easterlin et al., 2021). When detected and treated, CS and its sequela are preventable. However, preventing CS is complicated by missed opportunities to identify and treat both the mothers who have syphilis and their asymptomatic infants following delivery.
Neonates are most frequently infected with syphilis via vertical transmission, but exposure can occur through direct contact with genital lesions at delivery. During vertical transmission, the bacteria enters the fetal circulation directly, bypassing the primary stage of adult infection (Micheals, et al., 2018).
Signs and symptoms of infection from the dissemination of the bacteria to fetal organs and tissues can present in varying degrees of severity, ranging from no clinical indicators to critically illness. Manifestations of the symptoms of CS are divided into the time of occurrence. Symptoms of early congenital syphilis occur within the first 2 years of life, and symptoms of late congenital syphilis occur any time after that (Dobson & Sanchez, 2019).
Early Congenital Syphilis (Early CS)
The clinical indicators of early CS occur between birth and approximately 3 months of age, with most present within the first 5 weeks of life (Dobson & Sanchez, 2019). The most common symptoms include thrombocytopenia, hepatosplenomegaly, direct and indirect hyperbilirubinemia, rash, elevated transaminase levels, generalized lymphadenopathy, and anemia (Dobson & Sanchez, 2019; Esper, 2020; Michaels et al., 2018; Kollman & Dobson, 2016).
Late Congenital Syphilis (Late CS)
Symptoms of late CS are primarily the result of persistent inflammation (Dobson & Sanchez, 2019). The most common symptoms include Hutchison’s triad (eighth cranial nerve deafness, intestinal keratitis, and Hutchison’s teeth); frontal bossing; saddle nose; gummas of the viscera, skin and mucous membranes; rhagades; saber shins; and neurosyphilis (Dobson & Sanchez, 2019; Michaels et al., 2018; Esper, 2020; Kollman & Dobson, 2016).
Diagnosis
Syphilis is definitively diagnosed by direct visualization of spirochetes on dark-field microscope examination. However, several factors contribute to the limited availability of this technique in clinical practice. Obtaining accurate results depends on rapid access to the specimen, ideally within 20 minutes of collection, access to a dark-field microscope, and on the clinician’s ability to differentiate T. pallium from other normal flora spirochetes . Therefore, serologic testing is more commonly used (Collins Fantasia & McIntyre, 2019; Theel, Katz, & Pillay, 2020). Diagnosis of CS is challenging and multifactorial. Decisions for treatment are based on maternal infection status, adequacy of maternal treatment, neonatal clinical, laboratory, and radiographic findings, and comparison of maternal and neonatal NTT titers (Workowski et al., 2021).
The AAP (2018) has established guidelines for assessing maternal serologic findings and for neonatal evaluation criteria and treatment. The guidelines are summarized as follows:
PROVEN OR HIGHLY PROBABLE INFECTION
- Abnormal neonatal examination consistent with CS infection OR
- Neonatal NTT titer fourfold higher than maternal NTT OR
- Positive dark-field test or PCR of lesion or body fluid
Recommendations for Further Evaluation
- CSF assays (VDRL/RPR, cell count, and protein)
- CBC with differential and transaminases
- Radiographs of chest, long bones
- Neuroimaging
- Ophthalmologic examination
- Hearing examination
Recommendations for Treatment
- Preferred: aqueous crystalline penicillin G, 50,000 U/kg, IV, every 12 hours through 7 days of age, then every 8 hours beginning at day of life 8 for a total of 10 days of treatment
- Procaine penicillin G, 50,000 U/kg, IM, as a single daily dose for 10 days
POSSIBLE INFECTION
- Normal neonatal exam AND
- NTT titer equal to or less than fourfold maternal titer AND ONE OF THE FOLLOWING
- maternal treatment was inadequate (untreated or undocumented treatment) OR
- treatment received < 4 weeks before delivery OR
- alternative medication used for treatment
Recommendations for Further Evaluation
- If parenteral penicillin G is given for 10 days, further evaluation may be needed
- CSF assays (VDRL/RPR, cell count, and protein)
- CBC with differential
- Radiograph of long bones
Recommendations for Treatment
- Preferred: aqueous crystalline penicillin G, 50,000 U/kg, IV, every 12 hours for seven days, then every 8 hours for a total of 10 days of treatment
- Procaine penicillin G, 50 000 U/kg, IM, as a single daily dose for 10 days
- Benzathine penicillin G, 50,000 U/kg, IM, for one dose (only if evaluation, including CSF, is complete, values are normal, and follow-up is certain)
INFECTION LESS LIKELY
- Normal neonatal examination AND
- Neonatal NTT titer equal to or less than fourfold the maternal NTT titer AND
- Mother adequately treated before delivery AND
- No maternal signs of reinfection
Recommendations for Further Evaluation
- None
Recommendations for Treatment
- Preferred: Benzathine penicillin G, 50,000 U/kg, IM, for one dose
- Neonates of mothers with decreasing or low NTT titers may forgo treatment if followed every 2-–3 months until NTT becomes nonreactive.
- NTT titers should decrease by 3 months of age and be nonreactive by 6 months of age, but if titers are slow to decline or increase by 6–12 months of age, the infant should be evaluated and receive 10 days of medicinal treatment.
INFECTION UNLIKELY
- Normal neonatal examination AND
- Neonatal NTT titer equal to or less than fourfold the maternal NTT titer AND
- Mother adequately treated before pregnancy AND
- Maternal NTT titer low and stable before and during pregnancy and at time of delivery
Recommendations for Further Evaluation
- None
Recommendations for Treatment
- None, but if NTT is reactive at birth, the infant should be retested to ensure seronegative status is achieved
- Neonates with nonreactive NTT at birth but reactive maternal NTT should be retested at 3 months of age
- Benzathine penicillin G, 50,000 U/kg, IM for one dose (recommended by some)
Adapted from American Academy of Pediatrics (2018). Syphilis. In D. W. Kimberlin, M. T. Brady, M. A. Jackson, & S. S. Long (Eds.), Red book: 2018 report of the committee on infectious diseases (31st ed., pp. 773-787).
Neonatal care providers should be mindful that medication dosing is based on the infant’s chronological age, and dosing changes after 1 month of age. Also, if 1 day of treatment is missed, the entire 10-day course must be repeated. Antibiotics used for empiric therapy do not count as part of the 10-day course of treatment (Easterlin et al., 2021).
Follow-Up
Infants delivered to mothers who are seroactive at delivery should have repeat NTT testing every 2-–3 months until serology is nonreactive. Neonatal NTT titers should decline by 3 months of age and be nonreactive by 6 months. Evaluation and treatment are required if titers have not decreased or increased at 6–12 months following treatment. A positive cerebrospinal VDRL/RPR result at 6 months of age requires evaluation and treatment. A reactive NTT at 18 months confirms CS infection (Easterlin et al., 2021).
Syphilis and congenital syphilis are global health concerns, yet with proper testing and treatment of mothers and their babies, they are preventable. Maternal and neonatal care providers must remain knowledgeable and diligent in identifying and treating mothers and neonates with syphilis. Complete eradication of syphilis may be years into the future, but there is a lot that we can do now to decrease infection rates.
References
Adhikari, E. (2021). Syphilis in pregnancy: Diagnosis and treatment of ‘the great imitator’ that has resurged. Contemporary OB/GYN, 66(1), 22–27. https://www.contemporaryobgyn.net/view/syphilis-in-pregnancy
Adhikari, E. H. (2020). Syphilis in Pregnancy. Obstetrics & Gynecology, 135(5), 1121–1135. https://doi.org/10.1097/AOG.0000000000003788
American Academy of Pediatrics (2018). Syphilis. In D. W. Kimberlin, M. T. Brady, M. A. Jackson, & S. S. Long (Eds.), Red book: 2018 report of the committee on infectious diseases (31st ed., pp. 773–787).
Centers for Disease Control and Prevention. (2021a, April). Sexually transmitted disease surveillance 2019. https://www.cdc.gov/std/statistics/2019/default.htm
Centers for Disease Control and Prevention. (2021b, July). State statutory and regulatory language regarding prenatal syphilis screening in the United States. https://www.cdc.gov/std/treatment/syphilis-screenings.htm
Collins Fantasia, H., & MacIntyre, M. (2019). Syphilis update for women’s healthcare providers. Women’s Healthcare: A Clinical Journal for NPs, 7(3), 30–35. https://www.npwomenshealthcare.com/syphilis-update-for-womens-healthcare-providers
Dobson, S. R. & Sanchez, P. J. (2019). Syphilis. In J. Cherry, G. J. Harrison, S. L. Kaplan, W. J. Steinbach, & P. J. Hotez (Eds.), Feigin and Cherry’s textbook of pediatric infectious diseases (8th ed., pp. 1268–1284). Elsevier.
Our Sponsor


